10 Commonly Asked Questions About Uveitis

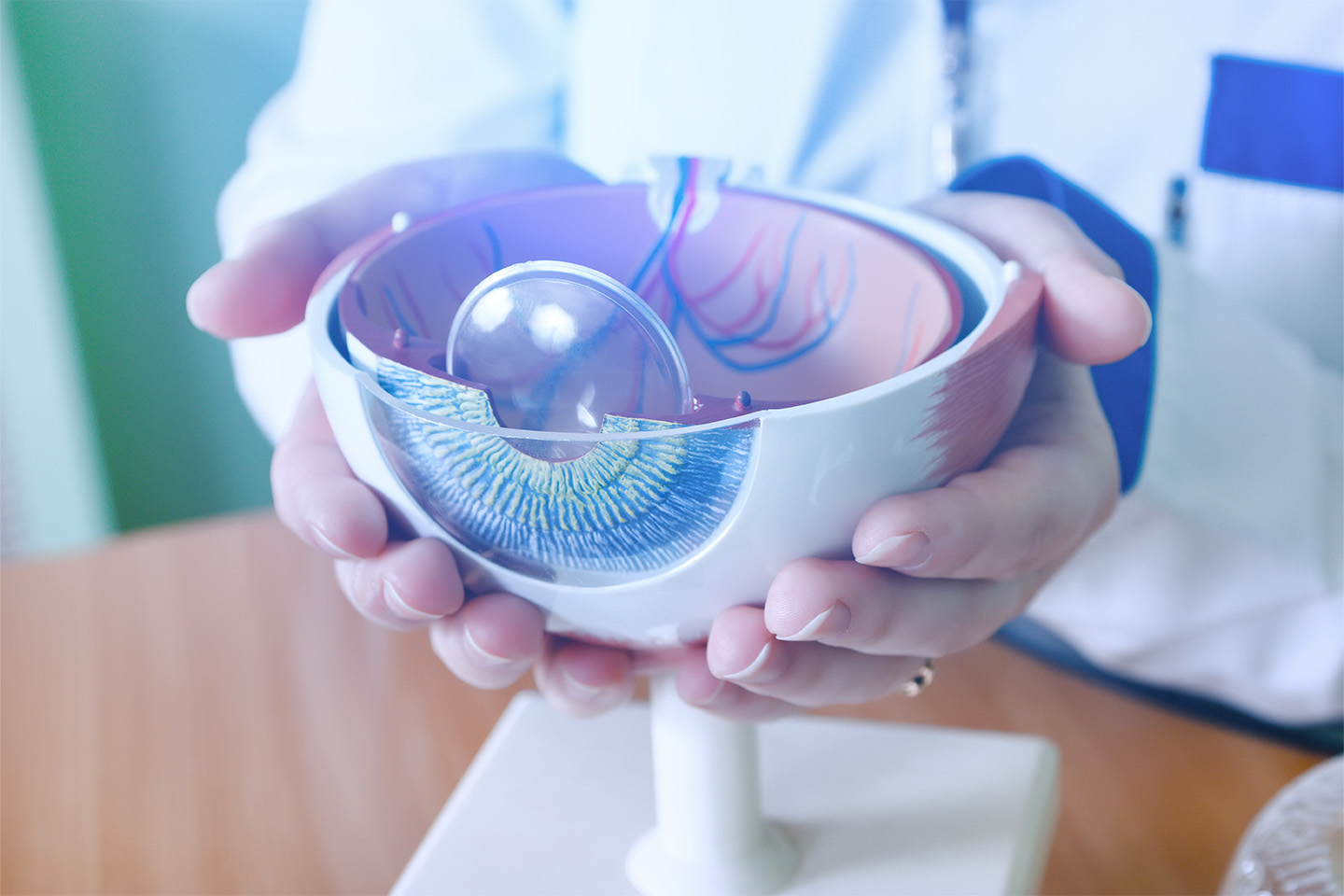
When your eyes start giving you trouble, the first thing you want to know is what’s causing the problem and whether it’s serious. Sometimes it’s easy to find the answer, but in some rare cases, the issue may be uveitis – the inflammation of the middle layers of the eye.
If you are suddenly experiencing the symptoms of this eye condition, including redness, throbbing pain, light sensitivity, floaters., then it’s important to get the information you need for swift and proper intervention.
Our skilled staff has compiled the 10 most commonly asked questions about uveitis to help you get started with treatment at Kleiman Evangelista Eye Centers of Texas.
1. Can uveitis be cured?
Uveitis can be cured with proper treatment. However, depending on the cause, it could take anywhere from weeks to months to resolve as the body continues to heal.
Unfortunately, in some cases, uveitis may recur or become chronic even after treatment.
2. Can uveitis go away on its own?
Some cases of acute uveitis will resolve on their own. Nevertheless, it is best to seek treatment from a professional. Left untreated, uveitis can severely damage the eye structures, leading to glaucoma, cataracts, and even permanent vision loss.
3. How do you get uveitis?
Uveitis is a direct result of the inflammatory response within the eye. When the body responds to infection, damage, or irritants by sending white blood cells to these tissues, it results in the heat, redness, and swelling that characterizes this condition.
4. How do you treat uveitis permanently?
Treatment options will address your current uveitis attack, but there is no guarantee it will act as a permanent solution. For many individuals whose symptoms are caused by autoimmune or inflammatory diseases, this condition may still return even with treatment. However, most cases are acute and only occur once.
5. What is the best treatment for uveitis?
Treatment for uveitis can vary based on the cause and location of your condition but will typically involve some combination of the following:
Medicated eye drops – If the condition affects the front of the eye, your doctor may prescribe eye drops, like corticosteroids, to treat the inflammation. This will be the case for most patients. Additionally, your eye doctor may give you eye drops that dilate the pupil to control the painful spasms in the iris and ciliary body.
Oral antibiotics or antiviral medications – These options are used in conjunction with eye drops when the disease is caused by an infection or virus in the eye.
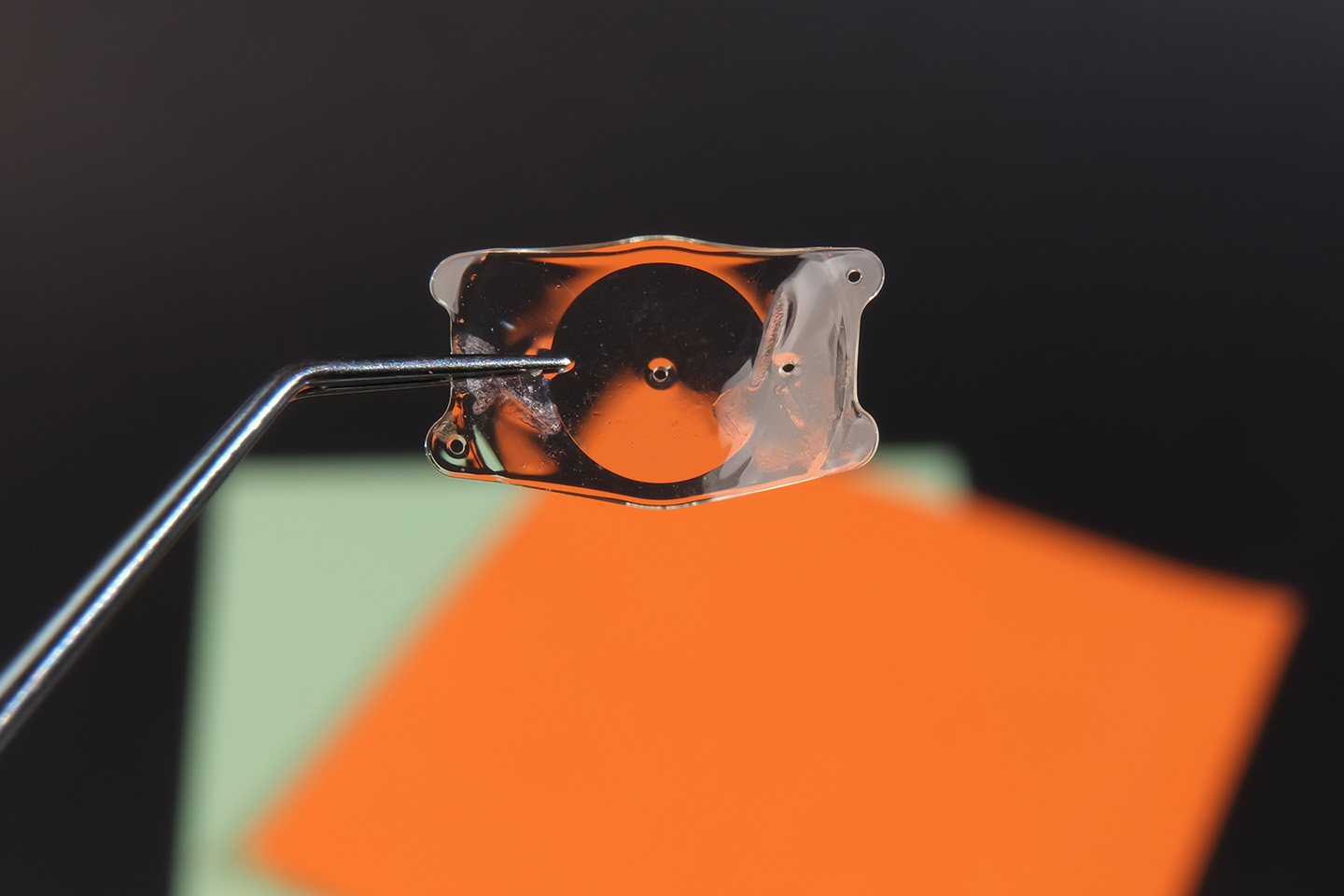
Corticosteroid injections or tablets – These options treat inflammation located in the posterior eye structures, like the retina, vitreous (gel-like fluid), optic nerve, or blood vessels. They may also be used if the inflammation is very severe. Corticosteroid injections might be used for short term control or long-term control as some steroid devices may last up to several months.
Immunosuppressants – These medications are meant to address the underlying autoimmune disease that may be contributing to your uveitis attacks.
6. What are the main causes of uveitis?
It is not always possible to pinpoint the direct cause of uveitis; however, some triggers include:
- Autoimmune or inflammatory diseases that can affect other parts of the body as well as the eyes, such as Crohn’s, sarcoidosis, lupus, rheumatoid arthritis, etc.
- Traumatic eye injuries
- Eye surgeries such as cataract and retinal detachment surgery
- Toxins
- Infections such as, like herpes, syphilis, toxoplasmosis, HIV, etc., or tumors in the eye (although this is rare)
- Side effects to medications (another rare occurrence)
There is some evidence that genetics could make you more susceptible to recurrent uveitis.
7. What causes uveitis to flare up?
If you have recurrent uveitis, then you are prone to flare-ups in times of high immune system activity. Of course, the common triggers mentioned above, such as infection, injury and inflammatory or autoimmune diseases, may cause flare-ups. Anecdotally, even seasonal allergies and stress can trigger another attack.
8. Is uveitis an emergency?
Uveitis can be considered a serious condition, especially if left untreated for more than a few days, but it is not usually an emergency. In cases of extremely painful red eye and elevated eye pressure, you should see your eye doctor immediately. They will be able to administer swift treatment to decrease the pressure and inflammation.
9. How do you test for uveitis?
Your eye doctor will conduct a thorough examination to determine whether you have uveitis, starting with an analysis of your medical history to rule out underlying factors.
From there, several tests will be conducted to confirm the existence, location and severity of your condition:
- Visual Acuity Test – Using the traditional eye chart, your eye doctor will test for changes to your vision.
- Tonometry – After applying numbing drops, your eye doctor will measure the intraocular pressure.
- Slit-Lamp Exam – A slit lamp shines a light into the eye to magnify and highlight the front structures and show inflammatory cells.
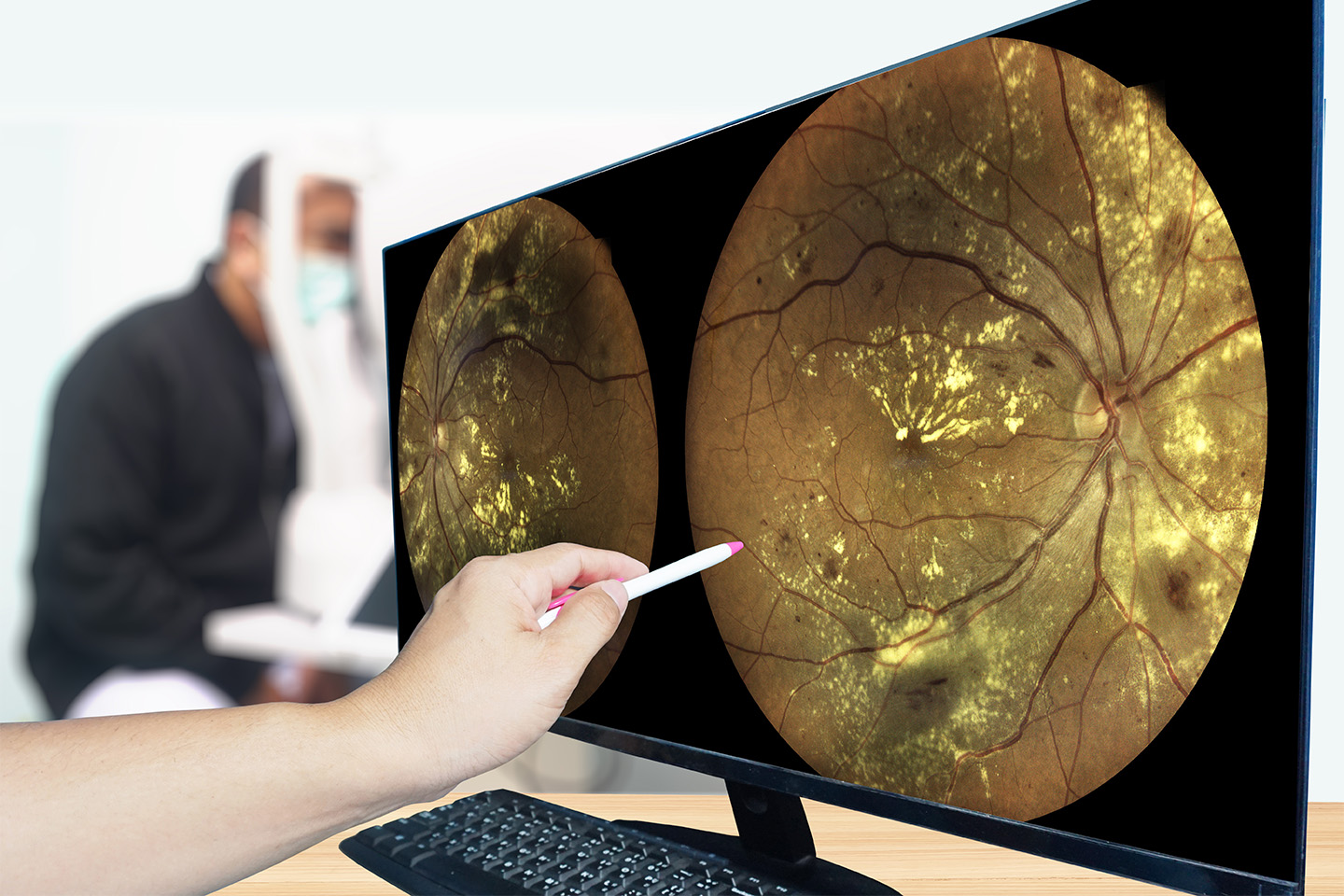
- Dilated Fundus Examination– This exam involves dilating your pupil and using magnifying lenses to shine a bright light and examine the middle and back of the eye. Dilating the pupil is also important in uveitis cases as it prevents permanent changes to the pupil from the inflammatory process.
Your eye doctor may want to conduct further imaging tests, including optical coherence tomography exams or MRIs. Blood work may also be ordered in recurrent cases to determine the cause of the uveitis. Concurrent treatment with a rheumatologist may be recommended in certain cases.
10. How long does uveitis take to heal?
Recovery time for uveitis can range from days to years, depending on the type (acute or chronic), location (anterior or posterior), and the effectiveness of the treatment option used. Your doctor can give you a more accurate timeline at the time of treatment.
The importance of getting comprehensive treatment for uveitis cannot be understated — and our specialized staff is here to get you started. Whether you are experiencing a mild case, or a lack of treatment has caused residual complications, we are prepared to help resolve your condition as experts in cataract and LASIK eye surgery in Dallas.